The Pancreas is a glandular organ located in the abdomen, positioned behind the stomach. It plays a crucial role in human physiology as both an Exocrine and endocrine organ.
Table of Contents
Definition of the Pancreas
The Pancreas serves as an Exocrine gland, producing and releasing pancreatic juices that contain enzymes essential for the process of digestion. Simultaneously, it functions as an endocrine gland, releasing hormones that regulate blood sugar levels, ensuring proper glucose homeostasis.
Importance of the Pancreas in Human Physiology
The Pancreas holds significant importance in the human body due to its dual functions. The enzymes produced by the Pancreas aid in the breakdown of carbohydrates, proteins, and fats, facilitating the efficient absorption of nutrients in the Small Intestine. Furthermore, the hormones secreted by the Pancreas play a vital role in regulating blood glucose levels, influencing energy metabolism, and supporting overall physiological balance.
This article aims to provide a comprehensive understanding of the Pancreas, covering its structure, functions and hormonal secretion. It deals with the Exocrine function of the Pancreas, i.e. the production and release of pancreatic juices, which contain enzymes important for digestion. It also discusses the endocrine function of the Pancreas, focusing on the release of hormones that regulate blood glucose levels.
The article also looks at the anatomical location of the Pancreas in the body, its blood supply and the different cell types within the Pancreas responsible for its specific functions. By examining the intricacies of the Pancreas, we can gain valuable insights into its vital contributions to human physiology and its role in maintaining overall health and well-being.
Pancreas Structure
Pancreas Location in the Body
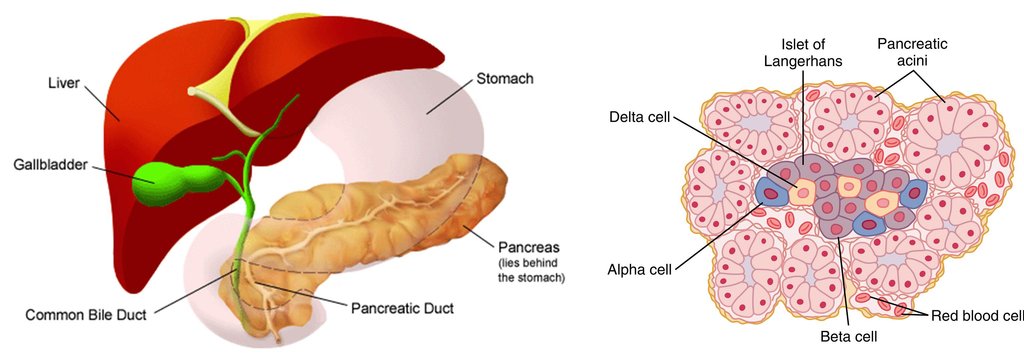
The Pancreas is situated in the abdominal cavity, specifically in the retroperitoneal space, behind the stomach. It extends horizontally across the upper abdomen, crossing from the left to the right side. The head of the Pancreas is nestled within the C-shaped curve of the duodenum, which is the first part of the Small Intestine. The body and tail of the Pancreas extend towards the left side, reaching the spleen.
External Appearance and Shape of Pancreas
The Pancreas has a somewhat elongated and flattened shape resembling a tadpole or a fish. It measures about 6 to 8 inches in length. The wider portion, known as the head, is located on the right side, while the tapering tail is positioned on the left side. The Pancreas exhibits a pale pinkish-grey colour, and its texture is relatively soft and spongy.
Pancreas Relations to Surrounding Organs
The Pancreas has anatomical relationships with several neighbouring organs. Anteriorly, it lies in close proximity to the stomach and the first part of the Small Intestine, the duodenum. Posteriorly, it is in contact with major blood vessels, including the superior mesenteric artery, the superior mesenteric vein, and the portal vein. The spleen is situated near the tail of the Pancreas, while the kidneys, adrenal glands, and the abdominal aorta are positioned behind it.
Microscopic Anatomy
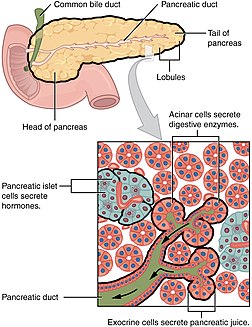
Pancreatic Lobules and Acini
At the microscopic level, the Pancreas is organised into small structural units called lobules. Each lobule contains numerous acini, which are clusters of secretory cells. Acinar cells are responsible for producing and releasing digestive enzymes into the pancreatic ducts.
Pancreatic Islets (Islets of Langerhans)
Scattered throughout the Exocrine portion of the Pancreas, there are specialised regions called pancreatic islets, also known as Islets of Langerhans. These islets are composed of different types of endocrine cells, including alpha cells, beta cells, delta cells, and PP cells. These cells play a crucial role in the endocrine function of the Pancreas by producing and releasing hormones directly into the bloodstream. For example, beta cells secrete insulin, while alpha cells produce glucagon.
Also Check – Also Check – Pancreatic Islet Transplantation
Pancreatic Ducts
The Pancreas contains a complex network of ducts that play a crucial role in the transport of pancreatic juices, which contain digestive enzymes and bicarbonate ions, from the Pancreas to the Small Intestine.
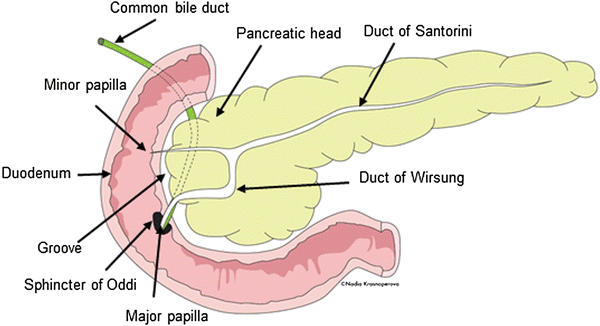
Main Pancreatic Duct (Duct of Wirsung)
The main pancreatic duct, also known as the duct of Wirsung, is the principal duct within the Pancreas. It runs through the length of the Pancreas, extending from the tail to the head of the organ. The main pancreatic duct collects pancreatic juices produced by the acinar cells within the pancreatic lobules and carries them towards the duodenum, the first part of the Small Intestine. It usually joins the common bile duct before emptying into the duodenum through the hepatopancreatic ampulla (also known as the ampulla of Vater) in the major duodenal papilla.
Accessory Pancreatic Duct (Duct of Santorini)
In some individuals, an additional duct called the accessory pancreatic duct, or the duct of Santorini, may be present. This smaller duct branches off from the main pancreatic duct and has its own separate opening into the duodenum through the minor duodenal papilla. The accessory pancreatic duct provides an alternative route for the transport of pancreatic juices and can act as a bypass if there is any obstruction or blockage in the main pancreatic duct.
The pancreatic ducts are lined with specialised epithelial cells that secrete bicarbonate ions and water into the pancreatic juice. Bicarbonate ions help neutralise the acidic contents from the stomach, creating an optimal pH environment for the action of digestive enzymes in the Small Intestine.
The intricate network of pancreatic ducts ensures the proper flow and delivery of pancreatic juices to the digestive system. This allows for the effective digestion and absorption of nutrients in the Small Intestine, contributing to the overall process of digestion and nutrient assimilation in the human body
Pancreas Function
Pancreas Function in Digestion
Role of the Pancreas in the Digestive System
The Pancreas plays a vital role in the process of digestion by producing and releasing pancreatic juices into the Small Intestine. These juices contain enzymes and other substances necessary for the breakdown and absorption of nutrients from food. The Pancreas works in conjunction with other digestive organs, such as the stomach and Small Intestine, to ensure efficient digestion and nutrient absorption.
Pancreatic Juice and Its Composition
Pancreatic juice is a clear, watery fluid produced by the Exocrine cells of the Pancreas. It contains a combination of enzymes and other substances that aid in the digestion of various macromolecules.
Pancreatic Enzymes
Amylase- Pancreatic amylase is an enzyme responsible for breaking down complex carbohydrates such as starch and glycogen into simpler sugars such as maltose and glucose. It acts in the Small Intestine, where it continues the digestion of carbohydrates initiated by salivary amylase in the mouth.
Lipase- Pancreatic lipase is an enzyme involved in the digestion of fats or lipids. It breaks down triglycerides into fatty acids and monoglycerides that can be easily absorbed by the Small Intestine. Lipase works in conjunction with other enzymes, such as bile salts produced by the liver, to facilitate lipid digestion and absorption.
Proteases- The Pancreas produces several proteases, including trypsinogen, chymotrypsinogen and procarboxypeptidase. These enzymes are secreted in their inactive form and activated in the Small Intestine. Trypsinogen is converted into trypsin by an enzyme called enterokinase, which is produced in the intestinal mucosa. Once activated, trypsin can further activate other proteases in the pancreas. The proteases break down proteins into smaller peptides and amino acids, facilitating their absorption by the Small Intestine.
Bicarbonate Ions and pH Regulation – In addition to enzymes, pancreatic juice also contains bicarbonate ions, which help regulate pH in the Small Intestine. The bicarbonate ions neutralise the acidic chyme (partially digested food) that enters the Small Intestine from the stomach. This alkaline environment created by the bicarbonate ions is necessary for the optimal functioning of the digestive enzymes so that they can work in their optimal pH range.
Also Check – What is the Function of the Digestive Enzymes ?
How Pancreatic Juice Aids Digestion in the Small Intestine?
When food enters the Small Intestine, the Pancreas releases pancreatic juice into the duodenum, the first part of the Small Intestine. The enzymes present in the pancreatic juice, such as amylase, lipase, and proteases, start breaking down complex carbohydrates, fats, and proteins, respectively. This process ensures the efficient breakdown of these macromolecules into smaller, more absorbable components.
The bicarbonate ions present in pancreatic juice help neutralise the acidic chyme from the stomach, creating an optimal pH environment for the digestive enzymes to function effectively. This pH regulation is crucial for the enzymatic activity and ensures the protection of the Small Intestine from the damaging effects of the acidic chyme.
Pancreas Function in the Endocrine System
In addition to its role as an Exocrine gland involved in digestion, the Pancreas also functions as an endocrine gland. The endocrine cells of the Pancreas, which are located in the pancreatic islets ( Islets of Langerhans), secrete hormones directly into the bloodstream. These hormones play an important role in regulating blood glucose levels and the general metabolic balance.
Also Check – Digestive Glands – Definition , Types and Functions
Hormones Secreted by the Pancreas
The pancreatic islets consist of different types of endocrine cells that secrete specific hormones. The main hormones secreted by the pancreatic islets are insulin, glucagon, somatostatin, and pancreatic polypeptide.
Insulin
Insulin is a hormone produced by beta cells within the pancreatic islets. It plays a crucial role in regulating blood glucose levels. When blood glucose levels rise, such as after a meal, beta cells release insulin into the bloodstream. Insulin acts on various tissues, such as muscle, liver, and adipose tissue, promoting glucose uptake and utilisation. It facilitates the conversion of glucose into glycogen for storage in the liver and muscles. Insulin also helps inhibit the release of glucose from the liver, promoting overall glucose homeostasis.
Glucagon
Glucagon is a hormone secreted by alpha cells within the pancreatic islets. It has the opposite effect of insulin and functions to increase blood glucose levels when they are too low. When blood glucose levels drop, such as during fasting or exercise, alpha cells release glucagon into the bloodstream. Glucagon acts on the liver, promoting the breakdown of stored glycogen into glucose through a process called glycogenolysis. It also stimulates gluconeogenesis, the production of glucose from non-carbohydrate sources like amino acids and fats. These actions raise blood glucose levels and help maintain a stable supply of glucose for the body’s energy needs.
Somatostatin
Somatostatin is a hormone secreted by delta cells within the pancreatic islets. It functions as a regulatory hormone, inhibiting the secretion of both insulin and glucagon. Somatostatin helps to regulate the balance between insulin and glucagon, ensuring that blood glucose levels remain within a normal range. It also inhibits the release of various gastrointestinal hormones, contributing to the regulation of digestion and nutrient absorption.
Pancreatic Polypeptide
Pancreatic polypeptide is a hormone secreted by PP cells within the pancreatic islets. Its exact function is not fully understood, but it is believed to play a role in regulating pancreatic Exocrine function, appetite regulation, and gastric emptying.
Pancreas and its Role in Blood Sugar Regulation
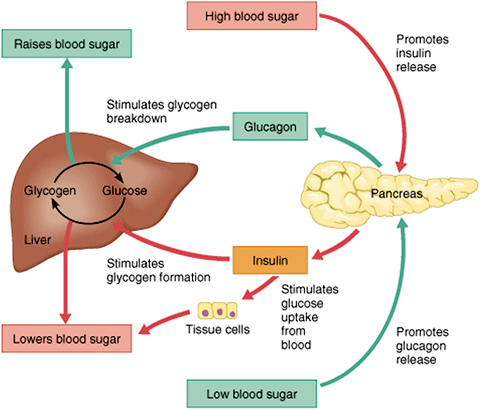
Insulin and Glucagon’s Interplay
The Pancreas plays a critical role in the regulation of blood glucose levels through the interplay of two key hormones- insulin and glucagon.
Insulin
Insulin is released by beta cells within the pancreatic islets in response to elevated blood glucose levels. Its primary role is to lower blood glucose levels by promoting the uptake and storage of glucose in various tissues, including muscle, liver, and adipose tissue. Insulin acts by facilitating the movement of glucose transporters to the cell membrane, allowing cells to take up glucose from the bloodstream. It also stimulates the conversion of excess glucose into glycogen through glycogenesis, promoting its storage in the liver and muscles. Insulin further inhibits the breakdown of stored glycogen (glycogenolysis) and the production of new glucose from non-carbohydrate sources (gluconeogenesis). Overall, insulin enhances glucose utilization, storage, and prevents the release of glucose from the liver, leading to a decrease in blood glucose levels.
Glucagon
Glucagon is produced by alpha cells within the pancreatic islets and acts in opposition to insulin. When blood glucose levels are low, such as during fasting or between meals, glucagon is released into the bloodstream. Glucagon stimulates the liver to break down stored glycogen (glycogenolysis) into glucose, which is then released into the bloodstream. It also promotes gluconeogenesis, the production of new glucose from non-carbohydrate sources like amino acids and fats. These actions increase blood glucose levels and provide a continuous supply of glucose to meet the body’s energy demands.
Regulation of Blood Glucose Levels
The Pancreas, through the coordinated action of insulin and glucagon, maintains blood glucose levels within a narrow range, a process known as blood glucose homeostasis.
Postprandial Phase
After a meal, blood glucose levels rise due to the digestion and absorption of carbohydrates. In response, beta cells of the Pancreas secrete insulin, which facilitates the uptake of glucose by various tissues, particularly muscle and adipose tissue. Insulin also promotes the storage of excess glucose as glycogen in the liver and muscles. This uptake and storage of glucose lead to a decrease in blood glucose levels, bringing them back to normal.
Fasting Phase
During periods of fasting or between meals, blood glucose levels decrease. In this state, alpha cells in the Pancreas release glucagon, which stimulates the liver to break down stored glycogen into glucose and promotes gluconeogenesis. These processes increase blood glucose levels, ensuring a constant supply of glucose to the body for energy production.
The precise regulation of blood glucose levels relies on a delicate balance between insulin and glucagon. Their interplay allows the Pancreas to respond to changes in blood glucose concentrations and ensure that glucose is available for cellular energy needs, maintaining overall metabolic balance.
Pancreatic Blood Supply
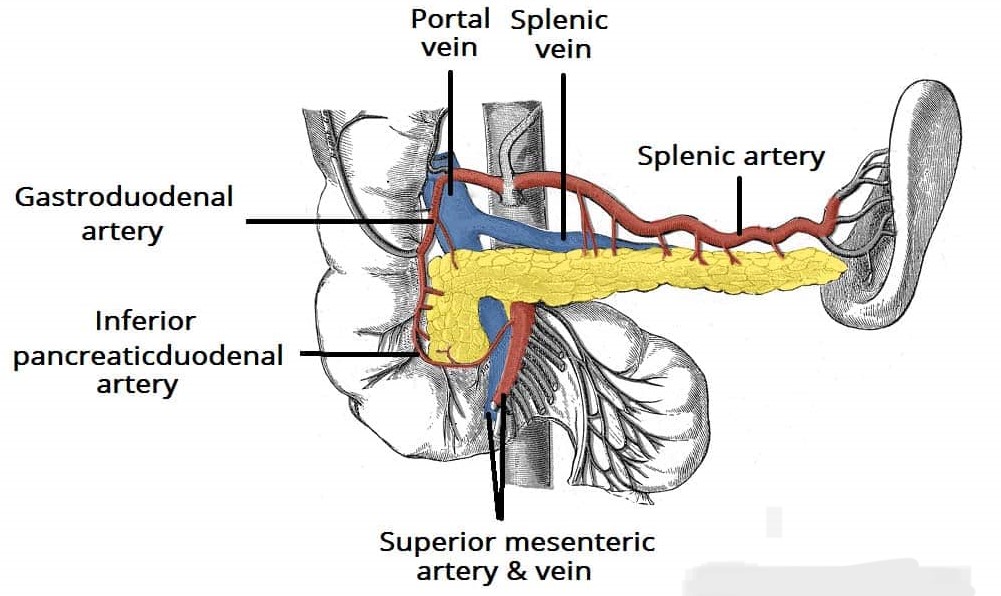
Arterial Supply of Pancreas
The Pancreas receives its arterial blood supply from several arteries, ensuring an adequate delivery of oxygen and nutrients to the organ.
Celiac Trunk
The celiac trunk, a major branch of the abdominal aorta, gives rise to the splenic artery. The splenic artery further branches into smaller arteries, including the short gastric arteries and pancreatic branches. These pancreatic branches supply the body and tail of the Pancreas with arterial blood.
Superior Mesenteric Artery
The superior mesenteric artery, another branch of the abdominal aorta, provides arterial supply to the head of the Pancreas through its pancreaticoduodenal arteries. These arteries form an anastomotic network with the branches of the splenic artery, ensuring collateral circulation within the Pancreas.
Other Arterial Contributions
In some individuals, additional arterial contributions may be present. These can include branches from the left gastric artery, gastroduodenal artery, or inferior pancreaticoduodenal artery, which arise from the superior mesenteric artery.
Venous Drainage of Pancreas
The venous drainage of the Pancreas follows a similar pattern to its arterial supply, with blood being drained into the systemic circulation.
Splenic Vein
Venous blood from the body and tail of the Pancreas is collected by the splenic vein. The splenic vein combines with the superior mesenteric vein to form the portal vein, which carries blood to the liver.
Superior Mesenteric Vein
The head of the Pancreas has venous drainage through its pancreaticoduodenal veins, which ultimately join the superior mesenteric vein. The superior mesenteric vein merges with the splenic vein to form the portal vein.
Other Venous Connections
The pancreaticoduodenal veins may have direct connections with other veins, such as the right gastroepiploic vein (draining into the superior mesenteric vein) or the gastric veins (draining into the portal vein).
The pancreatic blood supply ensures the delivery of oxygen and nutrients necessary for the normal functioning of the Pancreas. Arterial branches ensure proper perfusion, while venous drainage allows the removal of waste products and facilitates the transport of blood back to the systemic and portal circulations.
Pancreatic Diseases and Disorders
Pancreatic Diseases
Pancreatic diseases include a number of conditions that affect the structure and function of the pancreas. These diseases can have a significant impact on an individual’s health and require appropriate medical treatment. Some common diseases of the pancreas are-
Pancreatitis
Pancreatitis refers to inflammation of the pancreas. It can occur as acute pancreatitis or chronic pancreatitis. Acute pancreatitis is typically characterised by sudden and severe abdominal pain, often accompanied by nausea and vomiting. It can be caused by gallstones, excessive alcohol consumption, certain medications, infections or trauma. Chronic pancreatitis is a persistent inflammation that can cause long-term damage to the pancreas. Chronic alcohol abuse, hereditary factors, gallstones or autoimmune diseases can contribute to the development of chronic pancreatitis.
Pancreatic Cancer
Pancreatic cancer is a malignant tumour that originates in the cells of the pancreas. It is one of the most aggressive forms of cancer and has a relatively poor prognosis. Pancreatic cancer is often difficult to detect in its early stages because of its non-specific symptoms. It is commonly diagnosed at an advanced stage, which limits treatment options. Smoking, obesity, a family history of pancreatic cancer, chronic pancreatitis and certain genetic conditions are risk factors for pancreatic cancer.
Pancreatic Disorders
Pancreatic disorders specifically refer to conditions that disrupt the normal function of the pancreas. These disorders can affect the production and secretion of pancreatic enzymes and hormones and lead to various health complications. Some notable pancreatic disorders are –
Diabetes Mellitus
Diabetes mellitus is a chronic metabolic disorder characterised by elevated blood sugar levels. The pancreas plays a crucial role in diabetes by producing and regulating insulin, a hormone that helps control blood glucose levels. There are two main types of diabetes-
Type 1 Diabetes
This autoimmune condition occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little or no insulin, requiring lifelong insulin replacement therapy to manage blood sugar levels.
Type 2 Diabetes
In this condition, the body becomes resistant to the action of insulin and the pancreas no longer produces enough insulin to overcome this resistance. Lifestyle factors such as obesity, lack of exercise, poor diet and genetic predisposition contribute to the development of type 2 diabetes. Management typically involves lifestyle modifications, oral medications to improve insulin sensitivity or promote insulin secretion, and in some cases insulin therapy.
Other Pancreatic Disorders
Other disorders that can affect the pancreas include-
Pancreatic Exocrine Insufficiency
This condition occurs when the pancreas does not produce enough digestive enzymes, resulting in difficulty digesting and absorbing nutrients from food. It can be caused by chronic pancreatitis, cystic fibrosis or other pancreatic diseases.
Pancreatic Cysts
Pancreatic cysts are fluid-filled sacs that can form in the pancreas. Most pancreatic cysts are benign, but some can be precancerous or cancerous. They can be detected by imaging studies and may require monitoring or treatment depending on their size, location and characteristics.
Frequently Asked Questions on Pancreas
Question- What is the dual function of the pancreas?
Answer- The pancreas serves as both an exocrine gland, producing digestive enzymes, and an endocrine gland, releasing hormones that regulate blood sugar levels.
Also Check – Function of Pancreas
Question- Which part of the small intestine does the head of the pancreas connect to?
Answer– The head of the pancreas is nestled within the C-shaped curve of the duodenum, which is the first part of the small intestine.
Question- What is the external appearance and shape of the pancreas?
Answer- The pancreas has an elongated and flattened shape resembling a tadpole or a fish. It measures about 6 to 8 inches in length and has a pale pinkish-grey colour.
Question- Name one neighbouring organ that the pancreas is in contact with.
Answer- One neighbouring organ in contact with the pancreas is the stomach.
Question- What is the main function of acinar cells in the pancreas?
Answer- Acinar cells are responsible for producing and releasing digestive enzymes into the pancreatic ducts.
Question- What are the names of the two main pancreatic ducts?
Answer- The two main pancreatic ducts are the main pancreatic duct (duct of Wirsung) and the accessory pancreatic duct (duct of Santorini).
Question- What is the role of bicarbonate ions in pancreatic juice?
Answer- Bicarbonate ions in pancreatic juice help neutralise the acidic contents from the stomach, creating an optimal pH environment for the action of digestive enzymes in the small intestine.
Question- What are pancreatic islets, and what hormones do they produce?
Answer- Pancreatic islets, also known as Islets of Langerhans, are specialised regions in the pancreas composed of different types of endocrine cells. Beta cells secrete insulin, while alpha cells produce glucagon, among other hormones.
Question- Name three enzymes present in pancreatic juice and their respective roles in digestion.
Answer- Three enzymes present in pancreatic juice are-
- Amylase- Breaks down complex carbohydrates into simpler sugars.
- Lipase- Digests fats or lipids into fatty acids and monoglycerides.
- Proteases (e.g., trypsinogen, chymotrypsinogen, procarboxypeptidase)- Break down proteins into smaller peptides and amino acids.
Question- How do bicarbonate ions in pancreatic juice contribute to digestion?
Answer- Bicarbonate ions in pancreatic juice neutralise the acidic chyme from the stomach, creating an optimal pH environment for the digestive enzymes to function effectively.
Question- Which part of the small intestine receives pancreatic juice?
Answer- Pancreatic juice is released into the duodenum, the first part of the small intestine.
Question- What hormone is responsible for lowering blood glucose levels, and where is it produced?
Answer- Insulin is responsible for lowering blood glucose levels and is produced by beta cells within the pancreatic islets.
Question- What hormone is responsible for increasing blood glucose levels, and where is it produced?
Answer- Glucagon is responsible for increasing blood glucose levels and is produced by alpha cells within the pancreatic islets.
Question- Name the hormone that inhibits the secretion of both insulin and glucagon.
Answer- Somatostatin, secreted by delta cells within the pancreatic islets, inhibits the secretion of both insulin and glucagon.
Question- What is the role of pancreatic polypeptide?
Answer- The exact function of pancreatic polypeptide is not fully understood, but it is believed to be involved in regulating pancreatic exocrine function, appetite regulation, and gastric emptying.
Question-What is the primary role of insulin in blood glucose regulation?
Answer- The primary role of insulin is to lower blood glucose levels by promoting the uptake and storage of glucose in various tissues.
Question-Which hormone is released by the pancreas to increase blood glucose levels?
Answer- Glucagon is released by the pancreas to increase blood glucose levels.
Question-How does the Pancreas regulate blood glucose levels in the postprandial phase?
Answer- In the postprandial phase, the Pancreas releases insulin to facilitate the uptake of glucose by tissues, promoting its storage as glycogen and lowering blood glucose levels.
Question-What are the two main types of diabetes, and how do they differ?
Answer- The two main types of diabetes are type 1 diabetes and type 2 diabetes. Type 1 diabetes is an autoimmune condition where the immune system attacks and destroys insulin-producing cells in the pancreas. Type 2 diabetes occurs when the body becomes resistant to insulin or doesn’t produce enough insulin.
Question-What is the function of pancreatic enzymes in digestion?
Answer- Pancreatic enzymes help break down macromolecules such as carbohydrates, fats, and proteins into smaller, more absorbable components during digestion.
Question-Name a pancreatic disease characterised by inflammation of the pancreas.
Answer- Pancreatitis is a pancreatic disease characterised by inflammation of the pancreas.
Question-How does the Pancreas receive its arterial blood supply?
Answer- The Pancreas receives arterial blood supply from the celiac trunk and the superior mesenteric artery, among other arterial contributions.
Question-What is pancreatic exocrine insufficiency, and what can cause it?
Answer- Pancreatic exocrine insufficiency is a condition where the pancreas does not produce enough digestive enzymes, leading to difficulties in digesting and absorbing nutrients. It can be caused by chronic pancreatitis, cystic fibrosis, or other pancreatic diseases.