Breathing is an involuntary process essential for life, where our bodies continuously inhale oxygen and exhale carbon dioxide. This article will dissect the mechanism of breathing, focusing on the lungs, the diaphragm, and other respiratory muscles involved. We’ll explore inhalation, the phase where air enters the lungs, and exhalation, when air is expelled. A clear understanding of these processes is crucial, as it reveals how our respiratory system functions to sustain life.
Table of Contents
The Basics of Mechanism of Breathing
Breathing is the involuntary process of moving air in and out of the lungs, allowing for gas exchange with the blood. This process is crucial for delivering oxygen to body tissues and removing carbon dioxide. The mechanism of breathing can be broken down into two primary phases-
- Inhalation (inspiration)
- Exhalation (expiration).
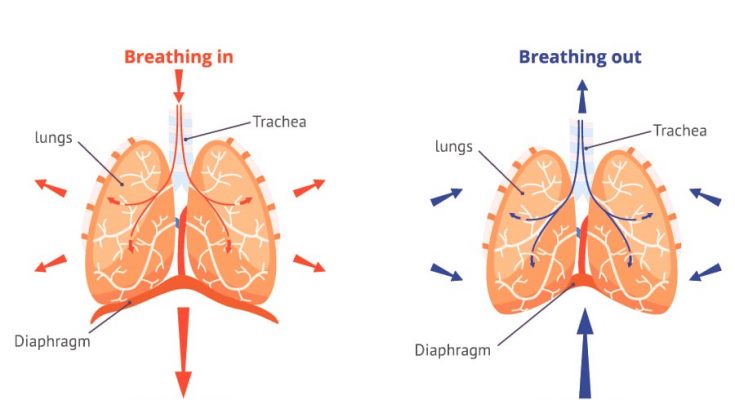
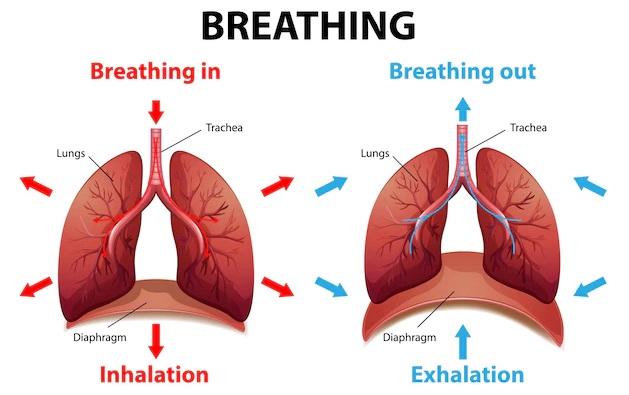
During inhalation, the muscles of the diaphragm and chest contract, expanding the thoracic cavity and decreasing the pressure within the lungs, drawing air in. During exhalation, these muscles relax, the thoracic cavity decreases in size, increasing lung pressure and pushing air out.
Difference Between Breathing and Respiration
While often used interchangeably in casual conversation, in scientific terms, breathing and respiration refer to two distinct processes. Breathing, as described, is the physical process of moving air in and out of the lungs. Respiration, however, refers to the biochemical process of releasing energy from nutrients, which occurs in every cell of the body. It involves the use of oxygen from the air to help break down glucose, releasing energy, water, and carbon dioxide as byproducts. Breathing is thus one component of the broader process of respiration, which includes not only gas exchange in the lungs but also the transport of gases by the blood to and from all cells of the body.
Overview of Key Components
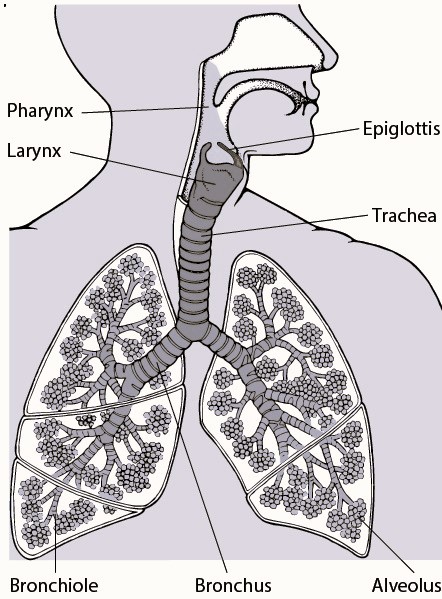
Several anatomical structures are crucial for the mechanism of breathing-
- Lungs- The primary organs of the respiratory system where gas exchange occurs. They expand and contract with the inhalation and exhalation of air.
- Diaphragm- A dome-shaped muscle located below the lungs that contracts and flattens during inhalation, increasing the thoracic cavity volume and decreasing lung pressure to draw air into the lungs.
- Intercostal Muscles- Muscles between the ribs that assist in expanding and contracting the chest cavity.
- Airways- Includes the nasal passages, pharynx, larynx, trachea, bronchi, and bronchioles, which air passes through as it moves in and out of the lungs.
- Alveoli- Tiny sacs within the lungs where the exchange of oxygen and carbon dioxide takes place, through the process of diffusion.
Inhalation- The First Step in Breathing Mechanism
Inhalation, or inspiration, is the active phase of the breathing cycle during which air is drawn into the lungs. It starts when the brain signals the respiratory muscles to contract, setting the stage for air intake. This process is vital for acquiring oxygen from the atmosphere, which is essential for our cells’ survival and functioning.
The Role of the Diaphragm and Rib Muscles During Inhalation
- Diaphragm- This dome-shaped muscle sits at the base of the chest and separates the thoracic (chest) cavity from the abdominal cavity. When you inhale, the diaphragm contracts and flattens, pushing the abdominal contents down and expanding the chest cavity vertically.
- Intercostal Muscles- Located between the ribs, these muscles assist in expanding the chest cavity. The external intercostal muscles elevate the ribs and sternum, further increasing the space within the chest.
As these muscles contract, they increase the volume of the thoracic cavity and decrease the pressure inside the lungs compared to the outside atmosphere. This pressure difference drives air into the lungs, filling the alveoli where gas exchange occurs.
How Thoracic Cavity Changes Facilitate Air Entry into the Lungs
The thoracic cavity is the space that houses the lungs and heart, bounded by the chest wall, spine, and diaphragm. During inhalation, the expansion of this cavity is crucial for creating the necessary vacuum that allows air to rush into the lungs. The mechanics involve-
- Volume Increase- As the diaphragm contracts and the rib cage expands, the volume of the thoracic cavity increases. According to Boyle’s law, an increase in volume leads to a decrease in pressure (when temperature is constant).
- Pressure Decrease- The increase in thoracic volume leads to a decrease in intrapulmonary pressure (the pressure within the lung alveoli). When this pressure is lower than the atmospheric pressure outside the body, air flows into the lungs.
- Air Entry- The air moves down its pressure gradient from the atmosphere into the lungs until the intrapulmonary pressure equalises with the atmospheric pressure.
Exhalation- Completing the Breathing Cycle
Exhalation, or expiration, is the phase of breathing where air is expelled from the lungs. It typically follows inhalation and is crucial in removing carbon dioxide, a waste product of cellular respiration, from the body. Unlike inhalation, exhalation is generally a passive process – meaning it doesn’t require muscular effort under normal, resting conditions. During exhalation, the diaphragm and intercostal muscles relax, leading to a decrease in the thoracic cavity’s volume. This decrease causes lung pressure to rise above atmospheric pressure, pushing air out of the lungs.
Differences Between Inhalation and Exhalation in the Breathing Mechanism
While inhalation is an active process involving muscle contraction to draw air into the lungs, exhalation is typically passive during relaxed breathing. Here are the primary differences-
- Muscle Activity- Inhalation requires the contraction of the diaphragm and external intercostal muscles to enlarge the thoracic cavity. In contrast, during exhalation, these muscles relax.
- Volume and Pressure Changes- Inhalation increases lung volume and decreases pressure, allowing air to flow into the lungs. Exhalation does the opposite – as lung volume decreases, pressure increases, and air is expelled.
- Energy Expenditure- Inhalation is energetically demanding due to muscle contraction. Exhalation requires minimal energy as it relies mostly on the elastic recoil of the lungs and thoracic cavity.
Mechanics Behind Lung Volume Changes During Exhalation
The change in lung volume during exhalation is primarily due to the relaxation of muscles. As the diaphragm relaxes, it moves upwards into a dome shape, and the intercostal muscles allow the rib cage to move downwards and inwards. These actions decrease the volume of the thoracic cavity. Because the lungs are elastic, they recoil and decrease in size as well. This increase in pressure inside the lungs compared to the atmospheric pressure drives the air out, completing the cycle of breathing.
Gas Exchange- The Core of Breathing Mechanism
In-depth Explanation of Oxygen and Carbon Dioxide Exchange in the Lungs
The primary function of the lungs is to facilitate the exchange of gases between the body and the environment. This involves taking in oxygen from the air and releasing carbon dioxide produced as a waste product from cells. The key site for this gas exchange is the alveoli, tiny air sacs within the lungs. Each alveolus is surrounded by a network of capillaries, small blood vessels that bring blood close to the thin alveolar walls. Oxygen from the air in the alveoli diffuses into the blood, while carbon dioxide diffuses from the blood into the alveoli to be exhaled. This exchange is driven by differences in concentration gradients, ensuring oxygen is supplied to the body and carbon dioxide is removed efficiently.
Significance of Alveoli in the Breathing Process
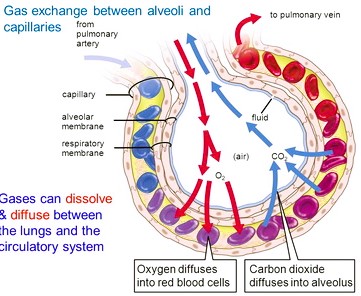
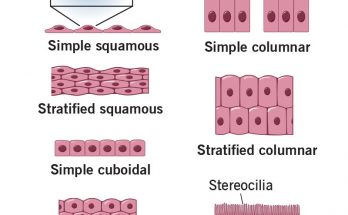
Alveoli are crucial in the breathing process due to their structure and function-
- Structure- Alveoli provide a large surface area relative to their volume, which maximises the area available for gas exchange. Their walls are extremely thin, allowing gases to move across them quickly.
- Function- Each alveolus is surrounded by capillaries, where the exchange of gases occurs. The elastic nature of the alveoli also aids in the efficient intake and expulsion of air with each breath.
The Concept of Diffusion in Respiratory Gas Exchange
Diffusion is the movement of molecules from an area of higher concentration to an area of lower concentration. In the context of respiratory gas exchange-
- Oxygen Diffusion- Oxygen molecules in the alveoli diffuse into the bloodstream because the oxygen concentration is higher in the alveoli and lower in the blood of the capillaries. This oxygen is then transported throughout the body via red blood cells.
- Carbon Dioxide Diffusion- Carbon dioxide, a waste product of cellular respiration, is higher in concentration in the blood than in the alveoli. Therefore, it diffuses from the blood into the alveoli and is expelled from the body during exhalation.
The efficiency of this diffusion process is critical for maintaining the body’s oxygen and carbon dioxide levels within a healthy range, which is vital for all cellular processes and overall health.
The Respiratory Gas Transport System and its Role in Breathing
The respiratory gas transport system is crucial for sustaining life, as it ensures the continuous exchange of oxygen and carbon dioxide between the lungs and the body’s tissues.
Oxygen Transport Mechanisms
Once inhaled into the lungs, oxygen passes into the alveoli and binds to haemoglobin in red blood cells, forming oxyhemoglobin. This compound transports oxygen through the bloodstream to body tissues. Here, influenced by factors like oxygen concentration and temperature, oxygen is released from oxyhemoglobin for use in metabolic processes.
The Function of Haemoglobin in Oxygen Transport
Haemoglobin, found in red blood cells, is key in oxygen transport. Each molecule can bind up to four oxygen molecules, enhancing blood’s oxygen-carrying capacity. Haemoglobin’s ability to efficiently bind and release oxygen is crucial, particularly under conditions like physical activity or stress, ensuring tissues have sufficient oxygen levels.
Mechanisms of Carbon Dioxide Transportation
Carbon dioxide, produced as a waste product in tissues, is transported back to the lungs via three mechanisms-
- Dissolved in Plasma- A portion dissolves in blood plasma.
- As Bicarbonate Ions- Most carbon dioxide reacts with water to form carbonic acid, which dissociates into bicarbonate and hydrogen ions. The bicarbonate ions are then transported in the plasma.
- Carbaminohemoglobin- Some carbon dioxide binds to haemoglobin, forming carbaminohemoglobin, which is transported to the lungs.
Circulation of Oxygenated and Deoxygenated Blood
- Oxygenated Blood- After picking up oxygen in the lungs, it is transported via pulmonary veins to the left side of the heart, then pumped to the rest of the body.
- Deoxygenated Blood- Post oxygen use, blood collects carbon dioxide and returns to the right side of the heart via veins. It’s then pumped to the lungs through the pulmonary artery for carbon dioxide removal.
Connecting Heart, Lungs, and Tissues
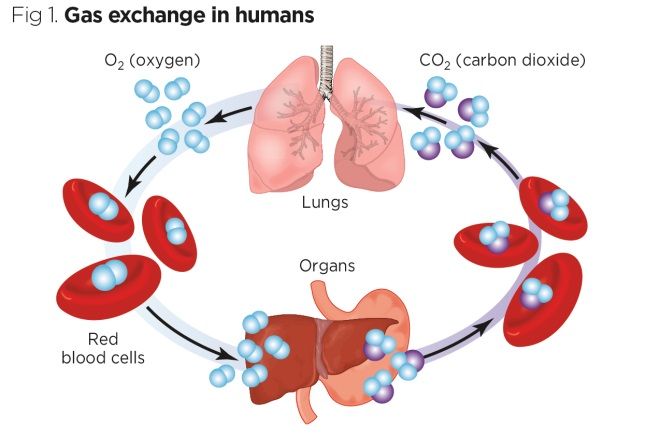
This cycle of oxygen and carbon dioxide transport is continuous and efficient. The heart, lungs, and tissues work together seamlessly-
- From Lungs to Heart- Oxygenated blood is pumped from the lungs to the left side of the heart.
- From Heart to Tissues- Oxygen is delivered to tissues, and carbon dioxide is collected.
- From Tissues back to Heart- Deoxygenated blood returns to the right side of the heart.
- From Heart back to Lungs- Blood is sent back to the lungs for gas exchange.
This process ensures a steady oxygen supply for the body’s tissues and the effective removal of carbon dioxide, maintaining bodily balance and health.
Why Do We Get Out of Breath When We Exercise?-Explained for Kids
Intrapleural Pressure- Role in the Breathing Mechanism
Intrapleural Pressure and Its Importance in Lung Function
Intrapleural pressure refers to the pressure within the pleural cavity, the space between the lungs and the chest wall. This pressure is crucial for proper lung function. Under normal conditions, intrapleural pressure is slightly negative compared to atmospheric pressure. This negative pressure is vital because it helps keep the lungs inflated and adhered to the chest wall. Without this negative pressure, the lungs would collapse due to their inherent elasticity.
Lung Expansion and Recoil in Relation to Breathing
During the breathing cycle, changes in intrapleural pressure play a significant role in lung expansion and recoil-
- During Inhalation- When we inhale, the diaphragm and intercostal muscles contract, increasing the volume of the thoracic cavity. This expansion leads to a further decrease in intrapleural pressure, creating a more negative environment relative to atmospheric pressure. The increased negative pressure allows the lungs to expand as they fill with air.
- During Exhalation- In contrast, during exhalation, the diaphragm and intercostal muscles relax, causing the thoracic cavity to decrease in volume. This decrease leads to a less negative intrapleural pressure, allowing the elastic properties of the lungs to initiate recoil. The lungs contract, pushing air out.
The concept of intrapleural pressure is essential in understanding how the lungs remain expanded and how they change volume during the breathing cycle. This pressure gradient between the intrapleural space and the atmosphere is a driving force for the mechanical process of breathing, facilitating the continuous movement of air in and out of the lungs.
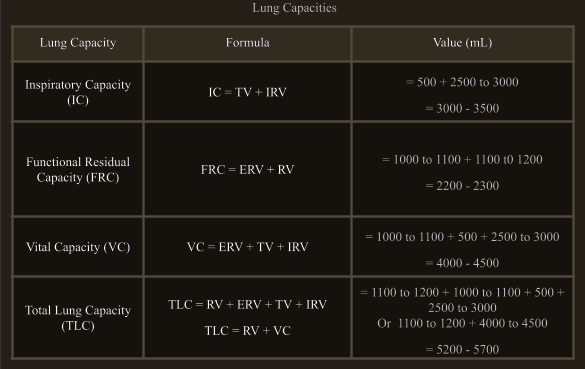
Lung Volumes and Capacities- Measuring Breathing Efficiency
Different Lung Volumes and Capacities
In respiratory physiology, lung volumes and capacities are essential in assessing the health and efficiency of breathing. These measurements offer insight into the functioning of the lungs and can be used to detect abnormalities. Lung volumes refer to the specific amounts of air that move in and out of the lungs during different phases of the breathing cycle, while lung capacities represent combinations of these volumes.
- Tidal Volume (TV)- The amount of air inhaled or exhaled during normal, relaxed breathing.
- Inspiratory Reserve Volume (IRV)- The additional air that can be inhaled with maximum effort after a normal inhalation.
- Expiratory Reserve Volume (ERV)- The additional air that can be exhaled with maximum effort after a normal exhalation.
- Residual Volume (RV)- The air remaining in the lungs after a forceful exhalation.
The Role of These Measurements in Assessing Lung Health and Breathing Efficiency
The combination of these volumes leads to various lung capacities, which provide valuable information for clinical assessment-
- Inspiratory Capacity (IC)- The total amount of air that can be inhaled after a normal exhalation (TV + IRV).
- Functional Residual Capacity (FRC)– The amount of air remaining in the lungs after a normal exhalation (ERV + RV).
- Vital Capacity (VC)– The total volume of air that can be exhaled after a maximal inhalation (IRV + ERV + TV).
- Total Lung Capacity (TLC)– The total volume of the lungs when filled with the maximum amount of air (TV + IRV + ERV + RV).
Key Concepts in the Mechanism of Breathing
Breathing, an essential life-sustaining process, involves two main phases – inhalation and exhalation. During inhalation, muscles like the diaphragm and intercostal muscles contract, expanding the chest cavity and allowing air to enter the lungs. Exhalation, typically a passive process, occurs when these muscles relax, leading to the expulsion of air from the lungs. This cycle is facilitated by the intricate design of the respiratory system, including the lungs, airways, and associated muscles.
Insights into Lung Elasticity, Surface Tension, and Boyle’s Law
Several key physiological concepts are crucial in understanding the mechanism of breathing-
- Lung Elasticity- The lungs possess inherent elasticity, allowing them to expand during inhalation and return to their original size during exhalation. This elasticity is vital for the efficient intake and expulsion of air.
- Surface Tension in the Alveoli- Within the alveoli, surface tension plays a significant role. The presence of surfactant, a substance that reduces surface tension, prevents the alveoli from collapsing and ensures that they can efficiently partake in gas exchange during each breathing cycle.
- Boyle’s Law- This physical law helps explain how changes in volume and pressure facilitate breathing. According to Boyle’s law, the volume of a gas is inversely proportional to its pressure. During inhalation, the increase in lung volume leads to a decrease in pressure, allowing air to flow into the lungs. Conversely, during exhalation, a decrease in lung volume leads to an increase in pressure, pushing air out.
The mechanisms of breathing involve a complex interplay between physical laws, biological structures, and physiological processes. The lungs’ ability to expand and recoil, the surface tension in the alveoli, and the principles of Boyle’s law all contribute to the rhythmic process of breathing. These concepts provide insight into how the respiratory system efficiently supplies oxygen to and removes carbon dioxide from the body.
In conclusion, the mechanism of breathing encompasses inhalation and exhalation processes, efficient gas exchange in the alveoli, and the transportation of oxygen and carbon dioxide in the body. Lung volumes and capacities play a crucial role in assessing respiratory health. Key concepts like lung elasticity, surface tension in the alveoli, and Boyle’s law are fundamental to understanding how the respiratory system functions to maintain the vital exchange of gases, essential for life.